Translate this page into:
Unusual clustering of comorbidities in a child with Down syndrome

*Corresponding author: Vrind Kumar Bhardwaj, Medical Director, Hormone Clinic, Wright Town, Jabalpur, Madhya Pradesh, India. vrind_b@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhardwaj VK. Unusual clustering of comorbidities in a child with Down syndrome. J Pediatr Endocrinol Diabetes. 2024;4:105-6. doi: 10.25259/JPED_11_2024
INTRODUCTION
Long standing, un-treated primary hypothyroidism in childhood is associated with changes in muscle and gonads.
CASE DESCRIPTION
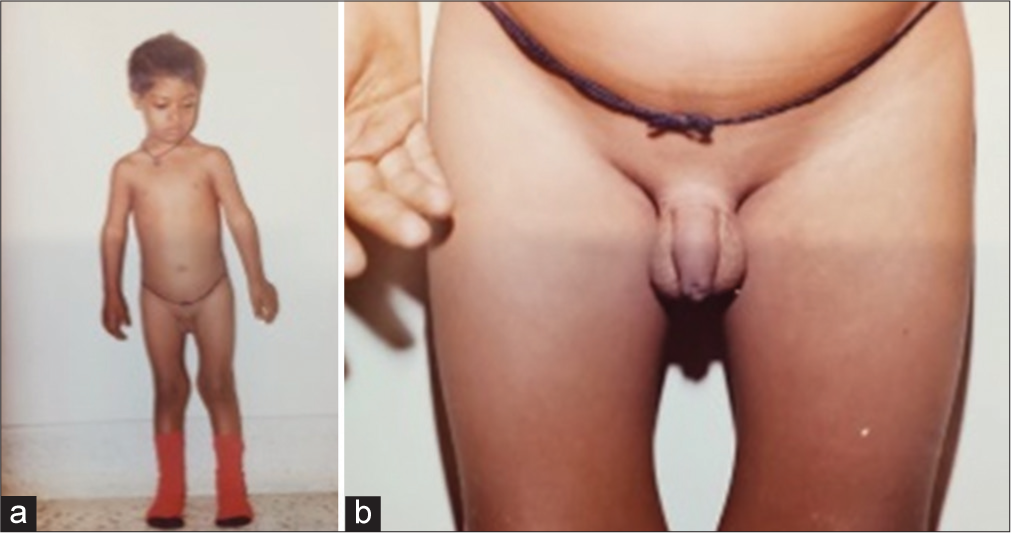
An 8-year-old child, karyotype confirmed case of Down syndrome, was referred for evaluation of lethargy and sleepiness. The child had clinical stigmata of Down syndrome. He was short (weight Z-score –2.58 and height Z-score –3.74). He had coarse facies with a depressed nasal bridge, a large tongue, dry skin, and a dull expression. His voice was hoarse. His movements were slow. The clinical picture was consistent with severe hypothyroidism. Muscles were bulky, particularly the calf muscles and thigh muscles, and firm on palpation [Figure 1a]. He had difficulty getting up from the floor with slowness of movements. He was unable to stand straight and kept his knees and hips partially flexed [Figure 1b]. He also had difficulty lifting his arms above head. His testes appeared to be large. His Tanner SMR staging was G2P1A1, testes were 5–6 mL in size (against normal pre-pubertal size of <4 mL) [Figure 1c]. The laboratory investigations showed the following: Hb 9.1 g/dL, total T4 <1.5 μg/dL, total T3 <40 pg/mL, TSH >100 mU/L, and anti-TPO antibody 86 IU/mL (normal <40), LH 0.3 IU/L, FSH 4.2 IU/L, testosterone <0.025 ng/dL, and creatinine phosphokinase (CPK) 350 U/L (normal up to 250 U/L). Skeletal maturation as per Greulich and Pyle Atlas was 4.5 years.

- 8-year-old boy with Down syndrome with primary hypothyroidism - pre-treatment: (a) Frontal view, (b) Bulky muscles, (c) Enlarged testes.
He was diagnosed with Down syndrome with hypothyroidism, myopathy (Kocher-Debre-Semelaigne syndrome) and peripheral pseudo-precocity (Van Wyk-Grumbach syndrome). He was started on treatment with levothyroxine 62.5 μg daily with other supportive measures. Follow-up after 3 months showed reduction in weight, increase in height, improvement in facies and skin with better movements, reduction in muscle bulk and reduction size of testes (3 mL both sides). Biochemistry showed reduction in CPK (104 IU/L) and improvement in thyroid hormone profile (total T4 6.5 μg/dL, total T3 102 pg/mL, and TSH 7.31 mU/L). The dose of levothyroxine was increased to 75 μg/day after 3 months. The changes in muscle and gonads were reversed by levothyroxine supplementation as seen in post-treatment pictures [Figures 2a and b].
- 8-year-old boy with Down syndrome with primary hypothyroidism - post-treatment: (a) Frontal view, (b) Testes.
DISCUSSION
The case study describes uncommon co-morbidities, hypothyroid myopathy and pseudo-precoicious puberty, in long standing untreated primary hypothyroidism in a child with Down syndrome.
CONCLUSION
Changes in muscle metabolism due to hypothyroidism lead to bulky and weak muscles. Primary hypothyroidism is associated with elevated TSH which can cross react with FSH receptor leading to precocious gonad activity.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.





